The problem with health teams
It’s difficult to build a “team” when the team doesn’t communicate to each other, often have no idea they’re on the team, and there is no common understanding of how each player contributes to your wellbeing.
I guess how I think of it is like this. Think of a team sport that you don’t the rules of, that’s the game we’re going to play. Now the players all know how to play the game, but you don’t. In your head, imagine all the players now blind folded, oh and make some of them deaf because they don’t listen to you. You’re the only one who can direct the game, but you don’t know the rules. Now play and try and win the game.
Does it sound familiar to you? This is what it feels like to me to have a chronic illness and my lived experience as a patient trying to navigate a health system and get all the treatment and care I need from across the different health and allied health disciplines.
So how do you fix it and make it work for you?
Tip 1: You’re the referee, captain and coach of your health team
It can be a big step to realise that only you can put you at the centre of your team and that you are the referee, captain and coach of that team. Everyone on the team wants what is best for you. But only you can make the decisions or ask questions. Only you can make complaints about your care. As Creaky Joints points out you need to raise your voice.
Small step for man, giant step for mankind. For some of us being in charge of our health team feels a bit like a giant step for mankind, but in reality it is a small step. It is a bit of mental gymnastics, but you can do it. You need to put yourself in the middle of the game, because you are unique. Only you know your body, what works for you and what is important to you. Health professionals can help you best if you are present and actively participating in the process.
If all the following information feels a bit overwhelming, no worries. You don’t have to do all of it all at once. It’s a bit of journey and you can build your team over time as you need and as priorities change and shift. Knowing that you’re in charge of the team is the most important step in helping you to organise a health team.
If its hard for you to raise your voice, what can you do?
You can find someone you know to support you. Or, you can go to a patient support organisation that focuses on your disease or injury. For example I work with Arthritis NZ because I have arthritis. But if you have a different type of illness you might approach a different organisation like MS Society, or, if you have a spinal injury, you might approach Spinal Trust NZ. Usually, but not always, these organisations have nurse educators or others who can help.
You can also look across your whole team, including your family and friends and see if there is someone there who can help you to raise your voice. You can take your voice-raisers to your consultations or just talk to them afterwards. They can help you prepare for your consultation.
Tip 2 Work out what you think will help you the most
To work out what you think will help you first need to educate yourself as much as you can stomach about your illness or condition. Take a break if its affecting your mood or bringing you down.
When you know a little more, then you need to work out what you think will help the most. Caring Ambassadors have good advice. They suggest having a good think about:
- what’s important to you
- what you think you need (ie pain management, etc)
- what might be possible gaps
- where do you think you will get the most benefit.
Working out what’s important to you is a critical part of building your health team because as Dr Ron Ehrlich says, disease and its treatment is expensive. Sometimes the providers, treatments, and supports are free and sometimes they’re partially funded and sometimes they’re not funded at all. You’ll need to prioritise based on what is most important to you. Be prepared to keep reviewing your priorities as your disease moves and shifts.
Tip 3 Once you have your priorities or goals, then build your team
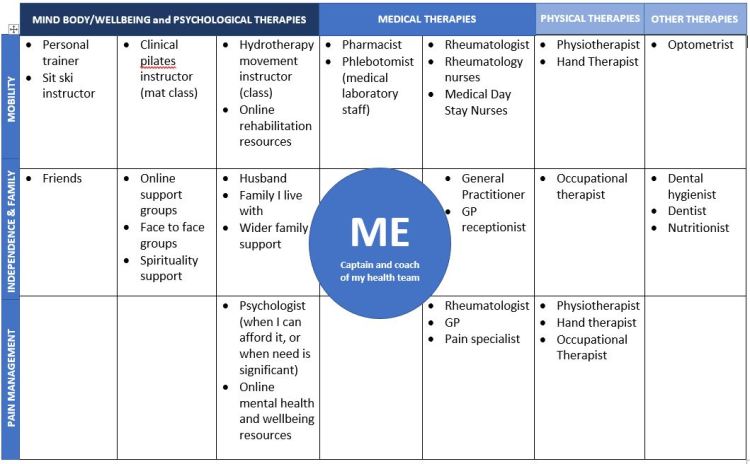
There can be a lot of people on your team. For example, if you have cancer there might be upwards of 23 people on your team. Diabetes care council list 14 people on their patient healthcare team. My team has 17 health professionals and other practitioners on it. My team also includes my family, friends and other groups that I belong to.
Tip 4 How do you find the right person / health professional?
There is a lot of personal cost in seeing people who can help you. You have to give your time, effort, money, and share your story which can be hard. The investment in the initial visit or consultation can feel big and might leave you not wanting to try someone else. That’s ok, its your choice. You’ll know you’re in sync with your team when you:
- have shared values – Mitchell and co
- honest,
- discipline,
- creativity (excited and motivated to tackle emerging problems creatively),
- humility (don’t see their training as superior to others),
- curiosity (want to keep learning)
- can reach them easily – A good location / accessibility for you, you can contact them electronically/digitally
- you like their bedside manner / treatment style
- don’t have to pay as much (if they’re covered by your plan for example in NZ they’re funded by ACC or are in the public health system)
- you are psychologically safe ie – they don’t make you cry
- they are proactive
Tip 5 getting the team to work well – coaching
- each practitioner will want to help you, that is everyone’s shared and common goals
- you need to tell each practitioner about your health team and who is on it
- but you need to understand their role and what they can do for you
- this understanding, plus learning your own information will help you to build mutual trust
- with greater trust it will be easier for you to ask questions and raise your voice
- you and your practitioner should be tracking your progress (Mitchell et al)
Tip 6 logistics are important to improving communication
- Consider access to shared records, tests, imaging. Bridging public and private systems makes communication more challenging, but not impossible
- I found when I was crossing private and public health care, I had to be much smarter about my health team and I had raise my voice even more
- Health passport
Tip 7 if you don’t get on with members of your team what can you do?
- Move on – the renegade nurse practitioners describes it as a bit like dating
- If you can’t move on, then
- participate as much as possible
- ask questions
- understand the role that your health team member plays and don’t expect too much of them. Some people are more comfortable staying with what they know, or the system supporting them might not be that great, they might have too many patients,
- Look across your team and bring in other team players from off the bench. For example:
- take someone you know to support you in your appointments
- Use your GP to write letters, or if urgent, pick up the phone and consult.
- Clinic nurses will help you to find the right question and to educate yourself. Clinic nurses will also write notes on your record.
Bibliography
Personal costs are time, effort, and money. Need your team members to collaborate with you (help solve problems, open share knowledge and are accountable, blending all the part that you and your team can offer to combine the most useful ideas into an effective plan to resolve your problem. Needs you to do it because health professionals don’t tend to work this way. Differing opinions, collaboration takes time, balance autonomy and compliance, recognise when you don’t need to collaborate, and let members of your team know about each other. GP, Support roles, knowing when to move on when the health practitioner is creating stress or not meeting your needs. Choosing a health care provided is like dating https://therenegadenp.com/blog/build-your-personal-healthcare-team
Look beyond drs, nurse, pharmacists, and other providers to incorporating evidence-based practices and lifestyle modifications that will add benefit. Ask yourself, which aspect of your health care do you want to address? What professionals exist to help, and then locate or find them. Really good slide on building an integrative care team at 2:03. Healing is process where wellbeing and quality of life is improved. They have 8 dimensions of health. Western medicine, Complementary medicine – Mind-Body therapies, body manipulation, exercise, energy therapies, creative therapies, nutrition and supplement, Nutrition – dietician or nutritionist, Exercise – physio, occupational therapist, exercise instructor, personal trainer, Stress, Wellbeing – awareness, connection, insight, purpose, Support system, spirituality what practices provide purpose and meaning. Has an integrative healthcare plan on 17:40. Right team for you – are they covered, are they easy to access, what is treatment style, will they support you and the rest of your team. Protect your health, don’t overlook. Step away if it is too hard. Ask questions, understand all aspects of your health conditions, listen to your body and trust your intuition, and be brave in all aspects of health. https://www.youtube.com/watch?v=ATYIR4flRK0&feature=youtu.be https://caringambassadors.org/after-a-diagnosis/build-your-healthcare-team/
Put yourself at the centre, Select a care coordinator (usually your GP), Choose health care providers who are good fit for you – someone you trust and believe in, respect and listen to you find an expert in your disease, become empowered you have to advocate for yourself, you can get a second opinion https://www.aamds.org/patients/control-your-care/build-health-care-team
Today’s Caregiver, build a list of all the people who can help you, include supports, plan a family meetings, play to strengths and consider family dynamics, then move out into health professionals and the others on your list https://caregiver.com/articles/building-care-team/
Creaky Joints guidelines – actively choosing your team will help you gain a better understanding of your condition, assess which treatments are right for you, and manage your health more effectively. Self-esteem and empowerment are two important skills for managing a chronic health condition. Think day to day – who supports you the most, then move out from there. Think health professionals, and allied health professionals, oral health optometrist, peer support groups. See if they know about AS, or if they’re prepared to research it. Trust, listens to you to, takes you seriously, and makes decisions with you. Rheum questions – condition progress, complementary therapies that would work, relevant support services available in your community and online. Raise your voice https://creakyjoints.org.au/pg/ https://creakyjoints.org/patientguidelines/
Cancer Support Community Factors to consider: past relationships, recommendations, expertise (do they know about your disease?), communication style, approach to treatment, availability of clinical trials, geographic location, insurance, urgent care needs Best way to be an advocate is to ask questions, access to the care team to ask question, what are the other options. 23 people on the cancer patient’s team https://www.cancersupportcommunity.org/article/your-cancer-care-team
Diabetes care team – Nice wheel diagram. You are the hub and everyone else is the spoke. https://www.thediabetescouncil.com/how-to-build-the-perfect-diabetes-care-team/
Canadian Diabetes Association – goals from GP and medication, pharmacist can tell more about medicine and side effects, community resources, diabetes educators and programme referrals, Make list, track goals, and keep notes http://guidelines.diabetes.ca/OrganizingCare/AngiesStory?_ga=1.89329051.1069657947.1475518908
Dr Liz Walker – You build your team, you hire them you fire them. Be empowered not making decisions out of fear or guilt. The best decisions are where there is alignment with your values. https://www.youtube.com/watch?v=Xc2KStyGzjE
Dr Ron Ehrlich Blog It’s not a quick fix have a chronic illness throw away the concept of quick fix and then go from there it’s a journey. It might take time and you will need to prioritise on the basis of finances or find work arounds. Think about what you feel needs improvement in your life and once you think about what is most lacking then start with that health professional. Self-care and self is at the heart https://drronehrlich.com/health-journey-lessons/
Team building in medical teams:
Team mission, team agreements, clarify team roles, and create team goals, learn from mistakes and failures, provide opportunities for the get to know each other
(abstract only) All team members understand, believe in and work towards the shared purpose of caring and working for patients. Openness and trust, with members working to their strengths, Teaming strategy to plan how people will act and work together, including effective use of communication technology https://pubmed.ncbi.nlm.nih.gov/26182585/
Evidence suggests that there are very few interventions to build teamwork in non-acute or ambulatory care setting. Tentative evidence that it can result in positive patient impacts. Given that the long term treatment of chronic disease represents an increasing burden on healthcare systems, this relative shortage of team training for non-acute setting represents an important gap to be addressed. Case loads are too large, or there is not enough shared care to warrant it. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-018-2961-9
Teams in GP small number of meaningful objectives, clear roles and responsibilities among team members, reflect on how the team is working together. Think about which roles you should recruit. Who do you need on your team and why? How can you get them to work together better – focus on their roles and think about how to build relationships, how proactive are your team, trust. How can you get your team to communicate effectively – do they have psychological safety? Can you speak up or they can talk to you about mistakes without retribution? All health professionals are accountable to you as a patient and to their regulator. Co-design is effective.
Values needed: honesty, discipline, creativity (excited and motivated to tackle emerging problems creatively), humility (don’t see their training as superior to others), curiosity (want to keep learning). Original reference Mitchell P, Wynia M, Golden R, McNellis B, Okun S, Webb CE, et al. Core Principles and Values of Effective Team-Based Health Care Discussion Paper. Washington, DC: Institute of Medicine; 2012. [Google Scholar]) and can be found here https://nam.edu/wp-content/uploads/2015/06/VSRT-Team-Based-Care-Principles-Values.pdf